Ever filled a prescription for a generic drug and been shocked at how much you paid-even with insurance? You’re not alone. In 2024, 42% of insured Americans reported paying more out-of-pocket for a generic medication than they would have if they’d paid cash at the pharmacy. That’s not a mistake. It’s how the system was designed.
Who’s really setting the price of your generic pills?
You might think your insurer sets the price of your generic drugs. Or maybe the pharmacy. But the real power lies with Pharmacy Benefit Managers, or PBMs. These are the hidden middlemen between drug manufacturers, insurers, and pharmacies. The three biggest PBMs-OptumRx, CVS Caremark, and Express Scripts-control about 80% of the market. They don’t just negotiate prices. They decide which drugs are covered, how much pharmacies get paid, and what you pay at the counter.Here’s how it works: when your doctor prescribes a generic drug like metformin or lisinopril, your insurer doesn’t pay the pharmacy directly. Instead, the PBM steps in. It has a secret list called the Maximum Allowable Cost (MAC), which tells pharmacies how much they’ll be reimbursed for that drug. This number is rarely based on what the pharmacy actually paid for the pills. Instead, it’s pulled from outdated benchmarks like Average Wholesale Price (AWP) or National Average Drug Acquisition Cost (NADAC)-both of which are manipulated by the industry to inflate numbers.
The hidden profit: spread pricing
The biggest twist? Spread pricing. This is when the PBM charges your insurer $50 for a generic drug, but only pays the pharmacy $10 for it. That $40 difference? That’s profit. And it’s not disclosed anywhere-not to you, not to your doctor, not even to most insurers. The Department of Labor estimates this practice generates over $15 billion a year in hidden revenue, mostly from generic drugs.Why does this matter? Because your copay is often based on what the PBM charges your insurer, not what the pharmacy actually paid. So even if the pharmacy bought the pills for $3, your insurance plan might be billed $45. And if your plan has a $45 copay for that drug? You pay $45. The pharmacy gets $10. The PBM pockets $35. And you’re left wondering why your insurance didn’t save you money.
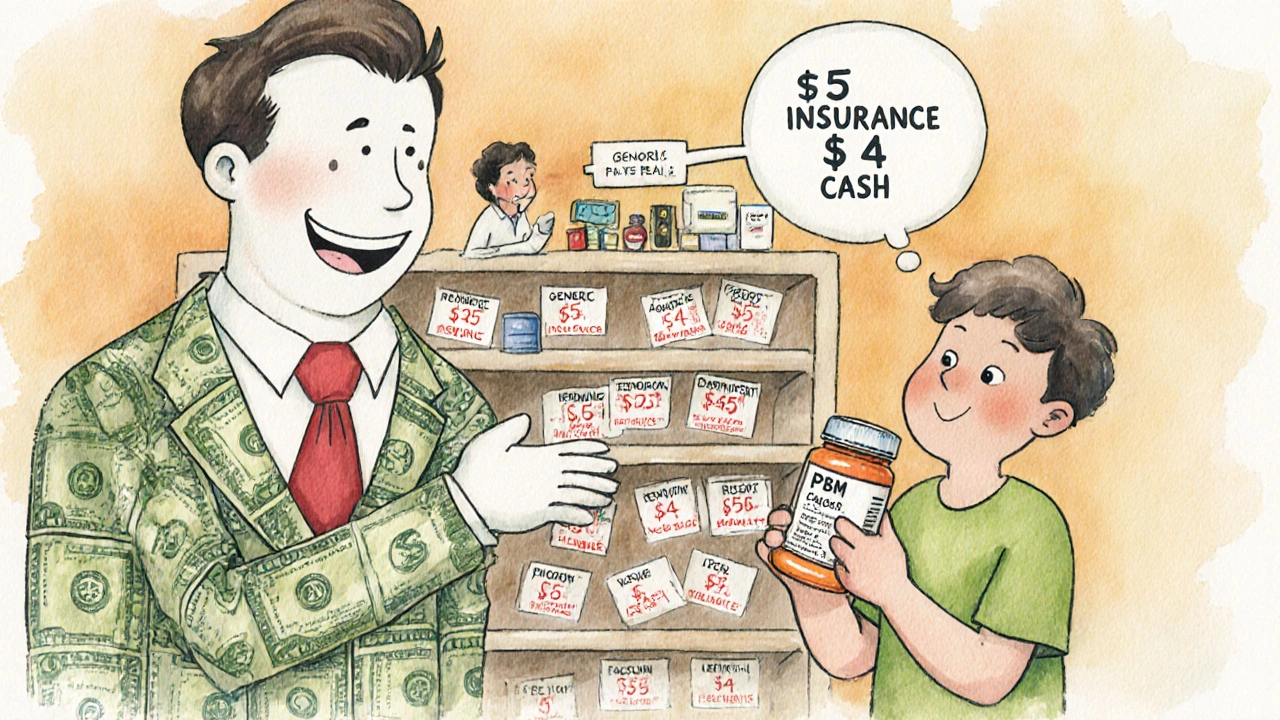
Why cash prices are often cheaper
This is why you’ve heard stories about people paying $4 for a 30-day supply of generic at Walmart or Costco-while insured patients pay $45. It’s not magic. It’s because those cash prices are based on the actual cost of the drug. The pharmacy pays $1.50, sells it for $4, and makes a small profit. No PBM. No spread. No hidden fees.But here’s the catch: pharmacists are often legally barred from telling you this. Ninety-two percent of PBM contracts include gag clauses that prevent pharmacists from informing patients about lower cash prices. It wasn’t until the No Surprises Act of 2020 that some of these clauses started being challenged. Even now, most patients have no idea they’re being overcharged.

How formularies control what you get
Your insurer’s formulary isn’t just a list of covered drugs. It’s a negotiation tool. PBMs pressure drug manufacturers to offer huge rebates in exchange for preferred placement on the formulary. The higher the list price, the bigger the rebate. So manufacturers inflate list prices to make rebates look impressive-and PBMs use those rebates to claim they’re saving money.But here’s the problem: your out-of-pocket cost is often tied to the list price, not the net price after rebates. So if a drug’s list price goes up, your copay goes up-even though the actual cost to the system may have dropped. Dr. Joseph Dieleman from the Institute for Health Metrics and Evaluation put it bluntly: “The current PBM system creates perverse incentives where higher list prices generate larger rebates, ultimately increasing patient cost-sharing burdens.”
Who pays the real price?
Independent pharmacies are getting crushed. Between 2018 and 2023, over 11,300 small pharmacies shut down. Why? Because PBMs pay them so little that many operate at a loss. Some pharmacies report being reimbursed $1.25 for a drug that cost them $3 to buy. Then, weeks later, the PBM does a “clawback”-taking back even more money after the claim was already paid. Sixty-three percent of independent pharmacists say clawbacks are common.On top of that, pharmacists spend 200-300 hours a year trying to decode PBM contracts. They need expensive software just to process claims correctly. And if a PBM changes its reimbursement rules overnight-something that happens in 41% of cases-pharmacists have no way to warn patients. Many are stuck with outdated systems, no training, and no recourse.

What’s changing-and what’s not
There’s pressure building. In September 2024, the Biden administration ordered PBMs to stop spread pricing in federal programs by January 2026. Fourty-two states are now passing laws to force transparency. The Inflation Reduction Act is starting to let Medicare negotiate drug prices, and experts believe that will push private insurers to follow.But the industry isn’t backing down. PhRMA, the drug lobby, argues that these negotiations threaten innovation. Meanwhile, McKinsey & Company predicts that PBMs will raise list prices to compensate for lost spread revenue. So even if spread pricing disappears, your copay might not.
What you can do right now
You don’t have to accept this system. Here’s what works:- Always ask the pharmacist: “What’s the cash price?”
- Use apps like GoodRx, SingleCare, or RxSaver to compare prices before you pay.
- If your copay is higher than the cash price, ask your insurer to adjust it-or switch plans.
- Check if your employer offers a transparent pharmacy benefit. Only 12% do, but they exist.
- Don’t assume insurance always saves you money. Sometimes, paying cash is the smarter move.
The system was built to look like it’s helping you. But for most people, it’s just making the cost of medicine more confusing-and more expensive. The truth is simple: if your generic drug costs less in cash than your insurance copay, you’re being overcharged. And you have the power to stop it.


Comments (11)
Kristi Bennardo
This is an absolute scandal. The PBM system is a legalized robbery scheme disguised as healthcare. I’ve paid $60 for a 30-day supply of metformin while my neighbor paid $4 cash - and the pharmacist couldn’t even tell me why. This isn’t capitalism - it’s corporate feudalism. Someone needs to go to jail for this.
Shiv Karan Singh
Lmao 😂 you think this is bad? In India, we pay $0.10 for generics and no one has insurance. You guys pay $45 for a pill that costs 2 cents to make? And you still say America is the best? 🤦♂️
Ravi boy
so like... pbms are just middlemen taking a cut? and pharmacists cant even tell you the cash price? wow. thats wild. i always thought insurance was supposed to help. turns out its just another layer of confusion. i just use goodrx now. its easier. 🤷♂️
Matthew Karrs
Let’s be real - this isn’t about PBMs. It’s about the Deep State using pharmaceutical pricing to control the population. You think your insulin cost is high? Wait until they start embedding microchips in the pills. The No Surprises Act? A distraction. The real agenda? Population reduction via medical debt. I’ve seen the documents. They’re not hiding it - they’re just waiting for you to stop asking questions.
daniel lopez
You people are so naive. PBMs didn’t create this mess - the government did. They allowed monopolies to form, then pretended to care. And now you’re mad at the middlemen? Wake up. The real villains are the politicians who took bribes from PhRMA and let this rot fester for 30 years. You want change? Stop voting for the same two parties. And stop blaming the pharmacists - they’re just trying to keep their jobs.
Nosipho Mbambo
...I... just... can’t... believe... this... is... happening... in... 2024...?!?!?!? I mean... I knew... insurance... was... broken... but... this... is... beyond... comprehension... I... have... a... 78-year-old... mother... who... pays... $80... for... blood... pressure... pills... and... she... doesn’t... even... have... a... smartphone... to... check... GoodRx... what... is... wrong... with... us...?
Katie Magnus
Ugh. I hate when people act like this is new. It’s been like this since 2010. Everyone’s just too lazy to care. I tried to tell my mom last year. She said, ‘But I have insurance!’ Like that’s a magic shield. Nope. It’s a trap. And now I pay cash for everything. No more ‘insurance’ nonsense.
King Over
cash price always lower if you dont have insurance or your plan sucks. i started using goodrx after i got charged 42 for lisinopril. paid 3.50 cash. same pill. same pharmacy. no magic. just greed
Johannah Lavin
Okay I just cried reading this. 😭 I work at a small pharmacy and I see this every single day. A grandma comes in with a prescription for $45 copay, I check GoodRx - it’s $3. I want to scream. But I can’t. Gag clause. I’m literally forced to lie by contract. I love my job but this system is soul-crushing. Thank you for exposing this. We’re not the villains - we’re trapped in it too.
Ravinder Singh
Bro this is why I moved to India for a year last time - I got my entire year’s supply of meds for $12. No insurance. No drama. Just pills. Back in the US, I pay $300/month for the same stuff. The system is rigged. But here’s the good part - you can fight back. Use apps. Ask for cash. Switch plans. Talk to your pharmacist. Even if they can’t say it out loud, they’ll nod and point to the GoodRx app. Small wins matter. Keep pushing. You’re not alone.
Russ Bergeman
Wait - so you’re saying the pharmacy gets paid less than the drug costs? And the PBM takes the rest? And the patient pays the inflated price? And pharmacists can’t even tell you? That’s... that’s... illegal? Right? Right?!?!?!? This isn’t just unethical - it’s fraud. Someone should sue. I’m filing a complaint. Right now. I’m not waiting.