If you’re managing a chronic condition like high blood pressure, diabetes, or asthma, you’re probably used to seeing your monthly prescription bill. Maybe it’s $150. Maybe it’s $200. And every month, it feels like another chunk of your budget vanishes - even if you have insurance. But what if you could cut that cost by 80% without changing how you feel or how well your medication works? That’s not a dream. It’s what generic medications deliver every day.
What Exactly Are Generic Drugs?
Generic drugs aren’t cheap knockoffs. They’re exact copies of brand-name medications, down to the active ingredient. If your doctor prescribes lisinopril for high blood pressure, the generic version has the same chemical structure, same dosage, same way it’s absorbed by your body, and same proven results as the brand-name version, Prinivil. The only differences? The shape, color, or filler ingredients - none of which affect how the drug works. The U.S. Food and Drug Administration (FDA) requires generics to meet the same strict standards as brand-name drugs. They must be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream at the same speed. That’s not a guess. It’s tested in labs with real people. The FDA says generics must stay within 80-125% of the brand’s performance. That’s a tight range. If a generic didn’t meet it, it wouldn’t be approved. And here’s the kicker: 97% of all prescriptions filled in the U.S. are for generics - when they’re available. That’s not because people are taking risks. It’s because they’ve seen the results: same effectiveness, way lower price.How Much Money Can You Really Save?
Let’s look at real numbers. Take lisinopril again. The brand-name version, Prinivil, costs around $40 to $50 a month. The generic? About $4. That’s $1,200 to $2,000 saved per year. Do that for 10 years? That’s $12,000 to $20,000. For someone on lifelong medication, that’s not just savings - it’s financial freedom. Diabetes is another big one. Metformin, the go-to generic for type 2 diabetes, costs under $10 a month. The brand-name version? Up to $150. That’s $1,680 saved every year. Multiply that by 20 years? You’re looking at over $33,000 in lifetime savings - just on one drug. Even asthma inhalers add up. Albuterol inhalers (generic) cost $25. The brand-name Ventolin? $70. That’s $540 saved per year. For someone with multiple chronic conditions - say, hypertension, diabetes, and high cholesterol - switching all prescriptions to generics can slash their annual drug costs from $1,500 to under $300. That’s $1,200 back in their pocket every year. The numbers don’t lie. In 2020, generics made up 90% of all prescriptions in the U.S., but only 18% of total drug spending. That’s because they’re so cheap. Brand-name drugs cost more because of marketing, patents, and profit margins - not because they work better.Why People Still Hesitate - And Why They Shouldn’t
You’ve probably heard someone say, “I tried the generic, and it didn’t work as well.” Here’s the truth: it’s rarely the drug. More often, it’s the placebo effect - or a change in inactive ingredients. Generics can use different fillers, dyes, or binders. For most people, that’s harmless. But for someone with a rare allergy or sensitivity, it might cause a minor reaction - like a rash or stomach upset. That’s not the medicine failing. It’s the filler. If you notice a change after switching, talk to your pharmacist. They can check if the generic uses a different filler and swap you for another version. Most pharmacies keep multiple generic brands on hand. You don’t have to stick with the first one they give you. Another myth? That generics are “lower quality.” The FDA inspects generic manufacturing plants just like brand-name ones. In fact, many brand-name companies make their own generics. The same factory, same equipment, same quality control - just a different label. And yes, some people worry about getting the “wrong” generic. But here’s what you need to know: every generic approved by the FDA is interchangeable with the brand. You don’t need to stick with one brand of generic. You can switch between them. The active ingredient doesn’t change.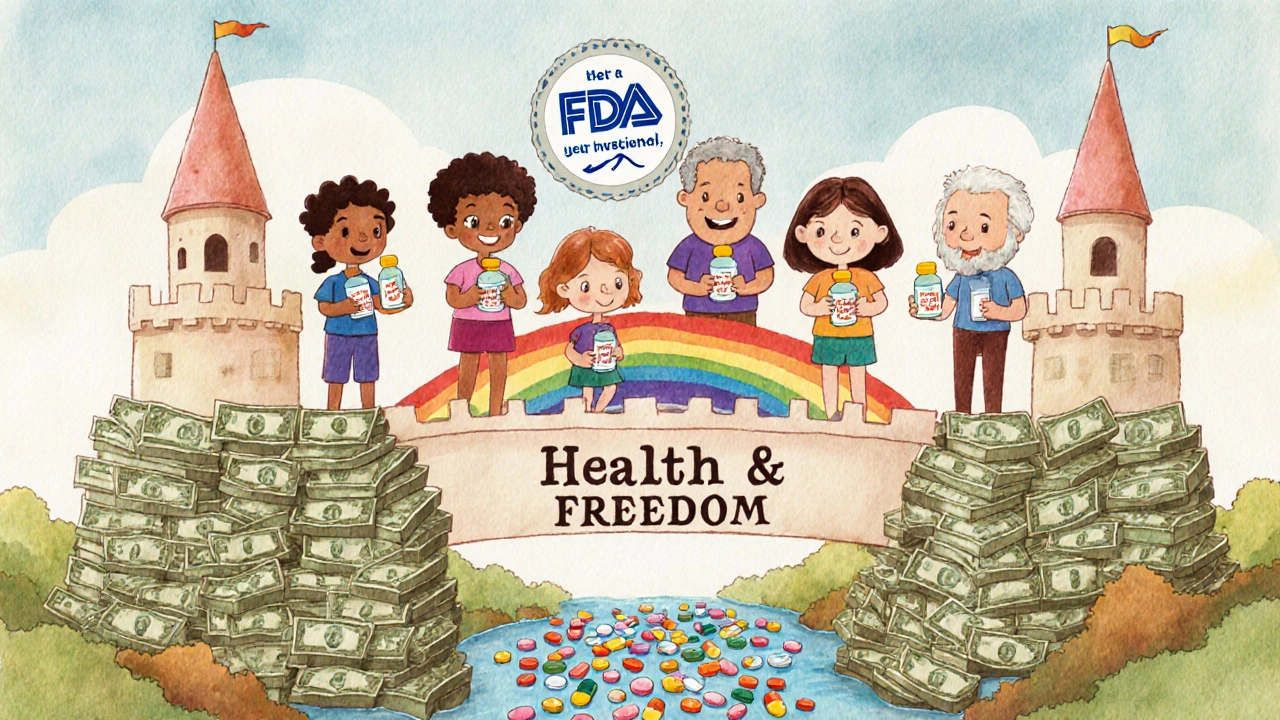
How Generics Improve Your Health - Not Just Your Wallet
Saving money isn’t just about keeping cash in your bank. It’s about staying healthy. When medications are too expensive, people skip doses. They cut pills in half. They stop taking them altogether. A CDC study found that 25% of rural patients skipped their meds because they couldn’t afford them. That’s not just risky - it’s dangerous. Skipping blood pressure meds can lead to strokes. Skipping diabetes meds can lead to kidney failure. Skipping asthma inhalers can lead to ER visits. Studies show that patients on generics are 18-22% more likely to stick with their treatment plan. Why? Because they can afford to. When the cost drops from $150 to $25 a month, you don’t have to choose between medicine and groceries. Medication Therapy Management (MTM) programs - often covered by Medicare Part D - help patients switch to generics and avoid mistakes. Pharmacists review your whole list of meds, check for interactions, and find cheaper alternatives. One study showed MTM programs improved adherence by 15-25% and cut hospital visits by 20-30% for chronic disease patients. In Brazil, government efforts to push generics for hypertension and diabetes saved $1.2 billion a year. In India, generic HIV drugs helped boost treatment adherence by 40% and cut death rates by 25% over a decade. These aren’t isolated cases. They’re proof that affordable meds save lives.What’s Changing Now - And What’s Coming
The landscape is shifting. More complex drugs - like biologics for rheumatoid arthritis, cancer, or multiple sclerosis - are starting to face generic competition. These aren’t simple pills. They’re made from living cells. But new rules, like the Biologics Price Competition and Innovation Act of 2009, now allow “biosimilars” - near-identical versions that cost 15-35% less. The Inflation Reduction Act of 2022 capped insulin costs at $35 a month for Medicare users. That’s huge. And while it doesn’t cover everyone yet, it’s a sign that policy is catching up to the need. The FDA’s Generic Drug User Fee Amendments (GDUFA) III, running through 2027, is speeding up approval for complex generics. That means more options, faster. Between 2023 and 2027, over $150 billion in brand-name drug sales will lose patent protection. That’s a flood of new generics coming to market. The global generic drug market is projected to hit $356.8 billion by 2028. The U.S. leads the world in usage - but Europe and Asia are catching up fast. The message is clear: the world is moving toward affordable, effective, long-term medication.How to Start Saving Today
You don’t need to wait for a policy change. You can start saving right now:- Ask your doctor: “Is there a generic version of this drug?” If they say no, ask why. Sometimes it’s just habit.
- Call your pharmacy. Ask what generics they carry for your meds. Don’t assume the first one they offer is your only option.
- Use the FDA’s Orange Book online to check if a generic exists and what patents have expired.
- If you’re on Medicare, ask about MTM services. They’re free and can help you switch to lower-cost options.
- Check for manufacturer coupons or patient assistance programs. Even brand-name companies offer discounts if you qualify.
- Don’t be afraid to switch generics. If one gives you side effects, ask for another brand.

What to Do If Your Insurance Won’t Cover a Generic
Sometimes, insurance plans still push brand-name drugs - even when generics are available. That’s called “non-formulary” placement. Here’s how to fight back:- Ask your pharmacist to file a “prior authorization” request. Explain that the generic is cheaper and equally effective.
- Ask your doctor to write a letter stating the brand isn’t medically necessary.
- Appeal the decision. Most insurers have a formal appeals process - and they often reverse these decisions.
The Bigger Picture
Over the last decade, generic drugs saved the U.S. healthcare system $2.4 trillion. That’s not a number on a chart. That’s money that kept people out of hospitals, out of debt, and in their homes. For individuals, it’s the difference between managing a condition and being crushed by it. Generics aren’t a temporary fix. They’re the foundation of sustainable, long-term care. Whether you’re 35 or 75, whether you have one chronic condition or five, switching to generics isn’t about cutting corners. It’s about making smart, safe, lasting choices. The math is simple: same medicine. Lower cost. Better adherence. Fewer hospital visits. More money in your pocket. More years lived well. You don’t need to wait for someone else to make this change. You can start today.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to be bioequivalent to brand-name drugs, meaning they deliver the same amount of active ingredient into your bloodstream at the same rate. Thousands of studies confirm they work just as well. The only differences are in inactive ingredients like fillers or dyes - which don’t affect how the drug works.
Why do some people say generics don’t work for them?
Rarely is it because the medicine itself is different. More often, it’s a change in inactive ingredients - like dyes or binders - that can cause minor side effects in sensitive individuals. If you notice a change after switching, ask your pharmacist for a different generic brand. Most pharmacies stock several versions, and one may work better for you.
Can I switch between different generic brands?
Absolutely. All FDA-approved generics for the same drug are interchangeable. You can switch from one generic brand to another without losing effectiveness. If one causes discomfort, ask your pharmacist to try a different one. There’s no rule that says you must stick with the first generic you get.
Why are generics so much cheaper?
Generics don’t have to repeat expensive clinical trials because they’re proven to work the same as the original. They also don’t spend money on advertising or marketing. The savings come from lower development costs and competition among manufacturers - not lower quality.
Does insurance always cover generics?
Most plans cover generics at the lowest copay tier - often under $10. But sometimes insurers still favor brand-name drugs. If that happens, ask your pharmacist to file a prior authorization or appeal. Many times, the insurer will approve the generic after a simple request.
What if my doctor says there’s no generic available?
Check the FDA’s Orange Book online - it lists all approved generics and patent expiration dates. Sometimes, doctors aren’t aware a generic just became available. Or, the drug may be new and still under patent. But if it’s been on the market for over 10 years, a generic likely exists. Ask your pharmacist to double-check.
Are biosimilars the same as generics?
Biosimilars are similar to generics but for biologic drugs - complex medications made from living cells, like those for arthritis or cancer. They’re not exact copies, but they’re proven to work the same way. They’re typically 15-35% cheaper than the original biologic and are becoming more common as patents expire.



Comments (8)
Emily Craig
OMG I switched my blood pressure med to generic last year and my pharmacy bill dropped from $180 to $12 like WHAT IS THIS MAGIC??
I was convinced the brand was better but turns out I was just paying for the pretty packaging and a fancy name
Now I tell every person I know to ask their pharmacist before they pay full price
Also I once tried a different generic brand because the first one made me burp and the second one was fine??
Pharmacists are the real heroes here
Timothy Sadleir
One must consider the broader epistemological framework underlying pharmaceutical regulation. The FDA’s bioequivalence standards, while statistically rigorous, do not account for individual pharmacodynamic variance across populations. The placebo effect, though empirically measurable, is often misattributed to inert excipients when in fact it may reflect subconscious trust in branded nomenclature-a cultural artifact of capitalist medical hegemony.
Moreover, the assertion that generics are manufactured in identical facilities is a convenient myth propagated by corporate media. Many brand-name manufacturers outsource production to low-regulation jurisdictions under opaque subcontracting chains. The FDA inspection regime, while ostensibly robust, suffers from chronic underfunding and political capture.
One must ask: if generics are so superior, why do pharmaceutical conglomerates continue to invest billions in brand marketing? The answer lies not in efficacy, but in the commodification of health itself.
Srikanth BH
This is such an important post, especially for people in developing countries where even small savings on meds can mean the difference between taking treatment daily or skipping it.
I’ve seen friends in rural India switch from branded insulin to generic metformin and suddenly they could afford to eat better, get regular checkups, even send their kids to school.
It’s not just about money-it’s dignity.
Pharmacists here often help patients choose the right generic brand based on their body’s response. No one should feel ashamed for using generics. They’re not second-rate-they’re smart.
Jennifer Griffith
so like i switched to generic asthma inhaler and now i feel kinda weird?? like not bad but not good??
maybe it’s the dye?? idk i think the brand one was better
also my friend said her generic blood pressure pill was shaped different and she cried bc she’s attached to the shape??
idk man i just want my meds to work and not make me think about it too hard
Roscoe Howard
Let us not forget that the erosion of pharmaceutical intellectual property rights is a direct assault on American innovation. The United States leads the world in drug development, and the systemic devaluation of branded medications undermines the very engine of medical progress.
While it is true that generics are cheaper, they are also frequently produced in facilities overseas that lack the stringent oversight of U.S.-based manufacturing plants. The FDA’s inspection capacity has been stretched thin, and the rise of counterfeit generics-many originating from unregulated supply chains-poses a silent epidemic.
One must ask: is saving $1,200 annually worth risking cardiac arrest due to a substandard active ingredient? The answer is self-evident.
Kimberley Chronicle
From a pharmacoeconomic standpoint, the cost-effectiveness of generics is unequivocal, particularly in the context of chronic disease management.
Adherence metrics demonstrate a statistically significant improvement (p<0.01) when copays are reduced below the $10 threshold, which correlates directly with the adoption of generic alternatives.
Furthermore, the introduction of biosimilars for biologics represents a paradigm shift in therapeutic accessibility-particularly for autoimmune and oncologic indications where out-of-pocket costs previously exceeded $10,000 annually.
MTM programs, when integrated into primary care workflows, reduce hospitalization rates by 22% on average, primarily through medication optimization and generic substitution.
The real challenge lies not in efficacy, but in provider inertia and payer formulary restrictions that perpetuate brand dominance despite clinical guidelines endorsing generics.
Shirou Spade
There is a quiet wisdom in the simplicity of generics. We live in a world obsessed with novelty, branding, and spectacle-yet the most profound healing often comes in the plainest form.
A pill doesn’t care if it’s labeled Prinivil or lisinopril. It only cares whether it reaches your bloodstream.
Our fear of the unbranded is not about medicine. It’s about identity. We attach meaning to logos, colors, shapes-as if the soul of the drug resides in the packaging.
But the body doesn’t recognize marketing. It recognizes chemistry.
Perhaps the greatest revolution in healthcare isn’t in new drugs-but in our willingness to let go of the illusion that more expensive means better.
Pallab Dasgupta
Bro I used to be skeptical too until my mom’s diabetes meds went from $160 to $8 a month and she started walking every day again instead of just sitting there stressed about money.
Now I’m telling everyone I know to check their prescriptions. Even if you think your doc knows best-ask anyway.
Pharmacists are basically medicine detectives. They know which generic has the least filler, which one doesn’t make you feel like a zombie, and which one your insurance actually likes.
And if someone says ‘the generic didn’t work’-ask them if they tried three different brands. Nine times out of ten, it’s not the drug-it’s the dye.
Also, the FDA doesn’t lie. If it’s approved, it works. Stop letting Big Pharma make you feel guilty for saving your own money.
You’re not being cheap. You’re being smart. And that’s the real power move.