When you're struggling to breathe, the last thing you want is to waste time figuring out how to use your medicine. Nebulizers and inhalers both deliver life-saving drugs straight to your lungs, but they work in very different ways. One looks like a small machine with a tube and mask; the other is a handheld spray canister. Which one should you use? And more importantly-which one actually works better?
How Nebulizers Work (And When They’re Necessary)
A nebulizer turns liquid medicine into a fine mist you breathe in through a mask or mouthpiece. It’s powered by a small air compressor that pushes air through a cup holding your medication. The mist particles are sized between 1 and 5 microns-just right to reach deep into your lungs. Treatment usually takes 5 to 15 minutes, depending on the machine and how much medicine you need.This slow, hands-off method is why nebulizers are still the go-to for babies, toddlers, and elderly patients who can’t coordinate breathing with pressing a button. If you’re having a severe asthma attack and can’t catch your breath enough to use an inhaler, a nebulizer lets you just sit still and breathe normally. That’s why emergency rooms and hospitals still keep them on hand.
But here’s the catch: most of the medicine never makes it to your lungs. Traditional jet nebulizers waste 60-70% of the dose. That’s because you’re breathing out while the machine keeps spraying. Newer breath-assisted nebulizers with one-way valves cut that waste down to 30-40%, but they’re more expensive and harder to find.
Another downside? Maintenance. Nebulizer cups and masks must be cleaned daily with warm soapy water and disinfected weekly with a vinegar solution. If you skip this, mold can grow inside-and inhaling mold spores is dangerous, especially if you’re immunocompromised. The CDC warns this is a real risk in home use.
How Inhalers Work (And Why Spacers Change Everything)
Metered-dose inhalers (MDIs) are small canisters that spray a precise dose of medicine when you press down. But here’s the problem: if you don’t time your breath right, most of the medicine hits your throat and gets swallowed. Without a spacer, only 10-20% of the dose reaches your lungs. The rest sits in your mouth, increasing the chance of thrush (a fungal infection) or hoarseness.Enter the spacer-a plastic tube with a chamber that holds the medicine after you press the inhaler. You breathe in slowly from the spacer, not the canister. This removes the need to coordinate pressing and breathing. Studies show that with a spacer, lung delivery jumps to 70-80%. That’s better than most nebulizers.
The American Thoracic Society says 70-80% of adults use inhalers incorrectly. That number drops to 5-10% when a spacer is used. And it’s not just for kids. Adults with COPD, severe asthma, or even those recovering from pneumonia benefit just as much. The Children’s Minnesota patient guide says: “Almost anyone-from infants to the elderly-can use a metered dose inhaler when it’s attached to a spacer.”
Which One Is More Effective? The Data Doesn’t Lie
You might think more medicine = better results. Nebulizers often deliver 2.5 to 3 times more total medication than an MDI with a spacer. But here’s what the science says: more medicine doesn’t mean better outcomes.A 2002 study by the American Academy of Family Physicians compared nebulizers and MDIs with spacers in emergency rooms. The results were clear:
- Patients using MDIs with spacers improved their peak airflow by 180 L/min-higher than the 145 L/min seen with nebulizers.
- They spent 50 fewer minutes in the ER (147 vs. 197 minutes).
- They needed less albuterol overall (8.4 mg vs. 12.6 mg).
- They had better blood oxygen levels and pH balance.
- Relapse rates at two weeks were half as high (12% vs. 28%).
Even the Global Initiative for Asthma (GINA 2022) recommends MDIs with spacers as the first-line treatment for most patients. Why? Because they work just as well, faster, and with fewer side effects.
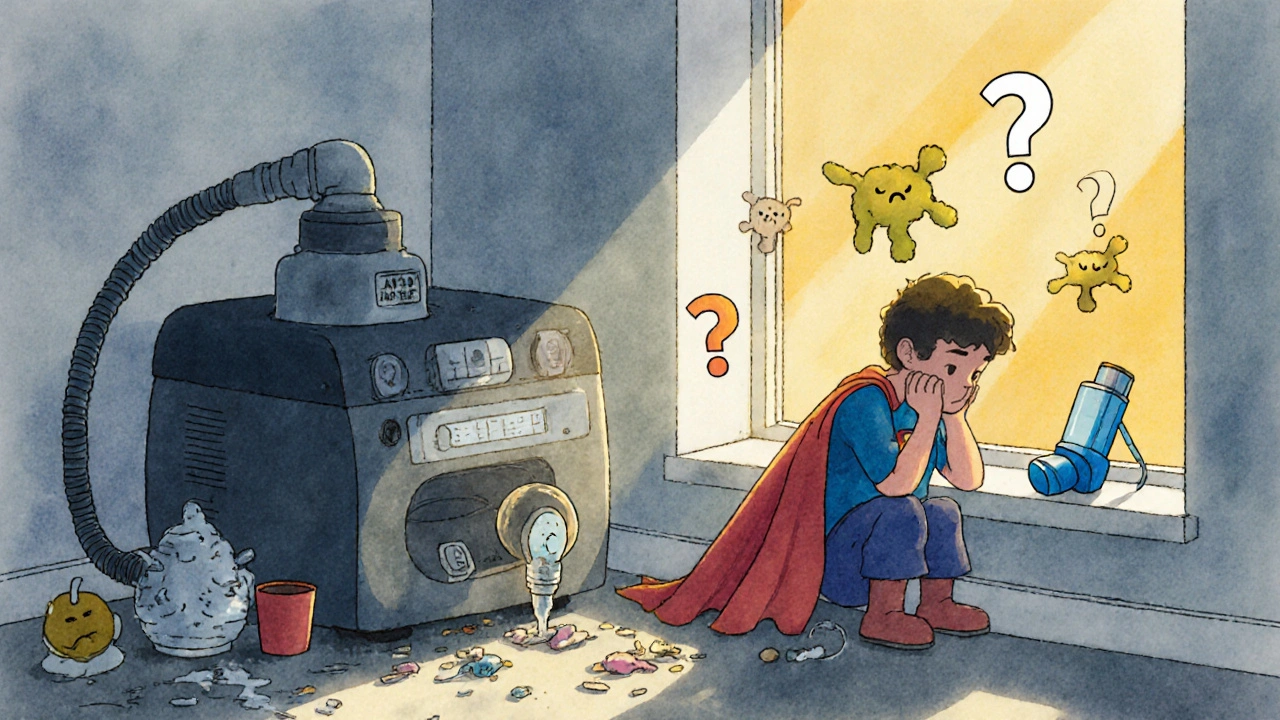
Why Do So Many People Still Prefer Nebulizers?
Despite the data, a 2022 survey of patients, doctors, and nurses found something surprising: 60.6% of patients believed nebulizers were more effective. Nearly half of doctors and nurses agreed-even though the evidence says otherwise.Why the disconnect? It’s psychological. With a nebulizer, you can see the mist, hear the machine hum, and feel the air on your face. It feels like something is happening. With an inhaler and spacer, you press a button, wait a second, and breathe in quietly. It feels too simple. One Reddit user wrote: “I used to use a nebulizer at home but switched to MDI with spacer-it cuts my treatment time from 15 minutes to 2 minutes and I can take it anywhere.”
Parents of young children often say they prefer nebulizers because “my child can’t hold still long enough to use an inhaler.” But that’s changing. Newer spacers come with fun designs, animal shapes, and even timers. Many pediatric clinics now train parents to use MDIs with spacers from age 1 up.
Cost, Portability, and Practicality
Let’s talk real life. A basic nebulizer system costs $100-$200. You need electricity. You can’t carry it in your purse. You can’t use it on a bus, at work, or while traveling. If you’re on a tight budget, you’ll also pay more over time-each nebulizer treatment uses more medication than an inhaler.An MDI with a spacer? A single inhaler costs $30-$50. Spacers are $10-$20 and last years. You can fit them in your pocket. You can use them anywhere. No cords. No noise. No waiting.
And then there’s infection risk. In hospitals, nebulizers are a known source of cross-contamination. One study found that cleaning them properly reduced infection rates by 70%. But at home? Most people don’t clean them well. Spacers? Wipe them once a week with a damp cloth. Done.
Who Should Use What? The Simple Guide
Here’s the bottom line:- Use a nebulizer if: You’re under 5 years old, have severe cognitive or physical limitations, are in acute distress and can’t coordinate breathing, or your doctor specifically recommends it during an emergency.
- Use an MDI with a spacer if: You’re over 5, able to breathe in slowly, want to save time, need to carry your medicine around, or want to reduce side effects and cost.
For most adults and older children, the MDI with spacer is the better choice. It’s faster, cheaper, safer, and just as effective. The only reason to stick with a nebulizer is if you physically can’t use the inhaler.
What About Dry Powder Inhalers (DPIs)?
You might hear about dry powder inhalers (DPIs)-devices that don’t use propellants and require a quick, strong inhale to release the medicine. They’re growing in popularity. The global market for respiratory devices is expected to hit $28.7 billion by 2028, with inhalers making up 65% of sales. DPIs now account for a big chunk of that growth.But DPIs aren’t for everyone. They require a forceful breath, which most young children and elderly patients with weak lungs can’t manage. If you’re not strong enough to blow out a candle in one breath, a DPI isn’t right for you. Stick with the MDI and spacer.
What’s Next? Smart Tech and Better Tools
The future of inhalers isn’t just about better design-it’s about smart tech. Devices like Propeller Health (now part of ResMed) track when and how often you use your inhaler. A 2022 study in JAMA Internal Medicine found that patients using smart inhalers reduced their rescue inhaler use by 58%. That’s huge.Researchers are also working on “device-agnostic” delivery systems-medicines that work the same no matter how you inhale them. But for now, the best tool is the one you’ll actually use correctly and consistently.
Can I use a nebulizer and an inhaler together?
Yes, but only if your doctor recommends it. Many people use a nebulizer for daily maintenance and an inhaler with spacer for quick relief during flare-ups. Others use an inhaler for everyday control and switch to a nebulizer only during severe attacks. Never combine them without medical guidance-overuse can lead to side effects like increased heart rate or tremors.
Is it safe to use a nebulizer every day?
It’s safe if you clean it properly and use it only as prescribed. Daily use is common for people with chronic COPD or severe asthma. But if you’re using it daily without a doctor’s direction, you may be overusing medication. Talk to your provider about whether an inhaler with spacer might be a better long-term option.
Do I need a prescription for a nebulizer or inhaler?
Yes. All asthma and COPD medications are prescription-only in the U.S. You also need a prescription to get insurance coverage for nebulizers or spacers. Over-the-counter inhalers exist, but they’re for temporary relief of mild symptoms and are not suitable for chronic disease management.
How do I know if I’m using my inhaler correctly?
Ask your doctor or pharmacist to watch you use it. Most people think they’re using it right, but studies show 70-80% of adults make mistakes. Common errors include pressing the inhaler too early or too late, not holding your breath after inhaling, or skipping the spacer. If you’re unsure, video yourself using it and compare it to a tutorial from the American Lung Association.
Are nebulizers better for children?
For kids under 5, yes-because they can’t coordinate breathing with pressing a button. But from age 5 and up, most children can use an inhaler with a spacer. Many pediatric clinics now teach kids to use spacers as early as age 2. Spacers are quieter, faster, and easier to clean than nebulizers, making them better for school and travel.
Can I travel with a nebulizer or inhaler?
You can travel with both, but inhalers with spacers are far easier. Nebulizers need electricity and are bulky. Most airlines allow inhalers in carry-ons without restriction. For nebulizers, check with your airline-they may require a doctor’s note. Always carry your inhaler with you, not in checked luggage. Cold temperatures can affect the spray mechanism.



Comments (6)
Ellen Sales
Okay, I just switched from my nebulizer to an MDI with a spacer last month-and I swear, it’s like waking up from a coma. No more 15-minute rituals. No more cleaning moldy cups. I can now use it on the subway, at my kid’s soccer game, even while walking the dog. And guess what? My asthma didn’t get worse. It got better. I’m breathing easier, spending less on meds, and honestly? I feel like I got my life back.
It’s not about the machine. It’s about the habit. If you’re still clinging to the nebulizer because it ‘feels’ more powerful, you’re not fooling your lungs-you’re fooling yourself.
giselle kate
Y’all are being ridiculous. The government and Big Pharma pushed inhalers because they’re cheaper. Nebulizers are the REAL treatment. You think some plastic tube with a button is gonna fix your lungs? That’s what they told us when they tried to replace insulin with pills. Wake up. The fact that hospitals still use nebulizers during emergencies tells you everything. This ‘spacer’ nonsense is just corporate propaganda dressed up as science.
And don’t even get me started on ‘smart inhalers’-next they’ll be tracking your breathing like it’s a TikTok trend.
Emily Craig
OH MY GOD. I just read this and I’m crying. Not because I’m sad-because I’m so mad I wasted 8 years using a nebulizer like it was some sacred ritual. I had a $150 machine collecting dust in my closet. I used to sit there like a robot, staring at the mist, thinking I was doing something profound. Meanwhile, my daughter was screaming because she couldn’t play outside after school. I didn’t know spacers existed until my pharmacist shoved one in my hand like, ‘Girl, you’re not a wizard. You’re just out of breath.’
Now we use the spacer. It’s silent. It’s tiny. It’s in my purse. And my daughter? She’s running track. I’m not crying because I’m emotional-I’m crying because I was so dumb for so long.
Karen Willie
Thank you for writing this. I’ve been a nurse for 18 years and I’ve seen so many patients-old, young, disabled, anxious-believe the nebulizer is the only way. It breaks my heart. I always show them the spacer. I let them hold it. I let them see how simple it is. And then I say, ‘You don’t need to suffer through a 15-minute chore to breathe better.’
Most people don’t realize that the spacer isn’t a ‘tool for kids’-it’s a tool for people who want to live their lives without being tied to a machine. If you’re using a nebulizer daily and you’re not in a crisis, ask yourself: Am I doing this because it works… or because I’m afraid to change?
Andrew McAfee
Just came back from visiting my cousin in Mexico. He’s been using a nebulizer since his COPD diagnosis 10 years ago. His wife cleans it with vinegar every week, like clockwork. But here’s the thing-he still gets sick more than I do. I use an inhaler and spacer. I’ve traveled to 12 countries. I’ve used it on planes, in hotels, even in the desert. I’ve never missed a day. I don’t need a power outlet. I don’t need to clean a cup. I just breathe.
It’s not about the tech. It’s about freedom.
Andrew Camacho
Let me break this down for you people who think this is a ‘debate.’
It’s not. It’s a scam. The entire respiratory industry is built on fear. Nebulizers are expensive. Spacers are cheap. Hospitals make more money when you’re in for 197 minutes instead of 147. Insurance companies push nebulizers because they’re reimbursed for the device AND the meds AND the cleaning supplies. And don’t even get me started on how many patients get billed for ‘home nebulizer therapy’ when they never even used it.
The science says MDI + spacer is better. But the system? The system wants you slow. It wants you dependent. It wants you cleaning that cup every damn week.
So yeah. Switch. But don’t think you’re just ‘getting better.’ You’re fighting a machine designed to keep you broken.